Best Running Shoes for Achilles Tendonitis: A Guide
Understanding the Achilles Tendon
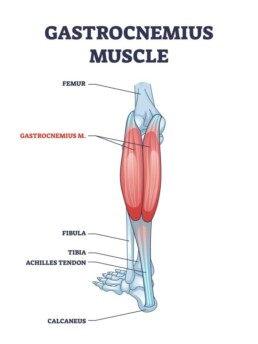
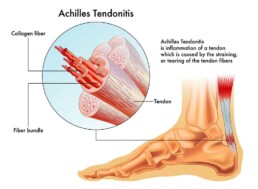
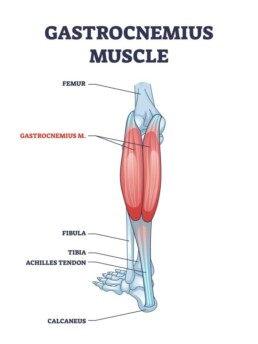
Tendons are the tissue fibres that connect the ends of our muscles to our bones. The Achilles tendon connects the major calf muscles – the gastrocnemius and the soleus – to the back of the heel. It helps us lift our heels off the floor and to push off when we run or jump. The tendon is named for Achilles, the man of ancient Greek legend whose mother held him by the heel to dip him into the River Styx to give him invulnerability – everywhere but the heel, which became his downfall in battle.
What is Achilles Tendonitis?
Achilles Tendonitis occurs when the tendon becomes swollen and painful and is caused by repetitive or intense strain. It is considered an overuse injury. Runners suddenly increase their workloads are subject to it, as are people who participate in sports only on weekends. Runners may also experience Achilles Tendonitis when they run too fast; tackle too many hills or those that are too steep; pronate as their feet strike the ground; or don’t take appropriate breaks between runs.
Different Types of Tendonitis
There are two types of Achilles Tendonitis: reactive and degenerative. Reactive Achilles Tendonitis is usually a response to a sudden increase in training load. A sufferer usually feels pain when beginning a run, but it will ease off as the run progresses, only to reappear afterward. On a scale of intensity, with 10 the worst pain, pain from this type of Achilles Tendonitis is usually a 3/10.
Degenerative Achilles Tendonitis or late disrepair is usually the result of ongoing overtraining and is generally seen in older runners. It results in changes to the tendon’s tissue – you may notice it thickening — and its ability to tolerate load. Without treatment, the tendon may be subject to rupture.
Be aware that the reactive type of Achilles Tendonitis may progress over time to degenerative tendonitis.
Is It OK To Run With Achilles Tendonitis?
As long as your Achilles Tendonitis remains in the reactive stage with pain that is a manageable 3 out of 10 and the symptoms subside a day after running, it is okay to continue your training, adapting based on the pain. However, if the pain becomes more severe and takes longer to subside, heed these warning signs. They are signals that your Achilles Tendonitis is moving from reactive to degenerative. Take a two week break from running and consult a licensed physiotherapist. It is probably time to focus on rehabilitation of your tendon, rather than on accumulating miles.
Once your physiotherapist tells you that you are ready to return to running, you’ll need to do so gradually. Overloading your tendon is what landed you in this situation in the first place, so increase your workload bit by bit.
If you do have reactive Achilles Tendonitis, you can generally keep running by adjusting your training plan. Rather than running daily or five times a week, alternate your running days with low-impact cross training – exercises such as cycling, swimming or rowing. These exercises will keep you fit without putting pressure on your tendon.
How Do I Stop My Achilles Tendon From Hurting When I Run?
When running with Achilles Tendonitis, be sure to start your workout sessions with at least 10 minutes of dynamic stretching to prepare warm up your tendon. Start by walking slowly and progressively increase the pace. You’ll help prevent pain once you begin to run.
As you plan your workouts, be conscious of the load your tendon is bearing and add to it gradually. Hill workouts and speed sessions may be detrimental if you aren’t careful, so reduce them or consider eliminating them until you heal.
As mentioned earlier, cross training is an ideal way to keep in shape and prepare your body for running. In addition to cycling, swimming or rowing, there are options such as Aquafit and exercises that strengthen your tendons, such as heel raises and plyometrics. Exercises for your hip muscles are also beneficial.
Finally, consider switching shoes. If your shoes have a heel stack of less than 10 millimetres, get a new pair (see below). If a new pair isn’t affordable, consider heel lifts to remove some of the pressure on your tendon.
Do Running Shoes Help With Achilles Tendonitis?
If you are suffering from Achilles Tendonitis, wearing the correct running shoe can help you manage it by reducing pain, increasing your capacity for running and assisting in overall rehabilitation. When shopping for shoes, select one with a deep heel cup, a rigid midsole and a stack drop of 10 millimetres (mm) or more. The deep heel cup helps to control your subtalar joint; when combined with a rigid midsole, it helps control pronation and relieve your tendon pain.
The heel stack refers to the running shoe’s difference in height between the back and front of the shoe. Research indicates that a raised heel helps relieve Achilles Tendonitis pain.
Shoe Fitting Guide for Different Foot Types
Consider these three shoes when you suffer from Achilles Tendonitis:
- Brooks Adrenaline. This running shoe offers stability. It has a 12 mm stack drop to help control Achilles pain and offers a moderate level of cushioning. Choose this model if you have mild Achilles Tendonitis symptoms and require moderate stability.
- Brooks Ghost 14. This shoe works for both running and the gym. The 12 mm stack drop shortens the Achilles and alleviates pain. It is useful for long distance runners experiencing mild to moderate Achilles pain.
- Asics Gel Kayano. This is a maximum stability shoe for road running. The deep heel cup and rigid midsole help control pronation, while the 13 mm stack drop relieves tension on the Achilles tendon. It is helpful for those with moderate to severe Achilles Tendonitis.
If you have any concerns or are seeking a more individualized workout plan, don’t hesitate to turn to your physiotherapist for guidance. It’s their job to help keep you moving – safely!
Rhomboid Pain
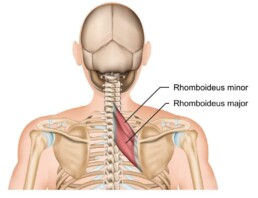
If you are feeling pain at the back of your neck between your shoulder blades and your spine, you may be experiencing rhomboid muscle pain. Before we delve into the pain itself, let’s identify the rhomboid muscles.
Your Rhomboid Muscles
Your rhomboid muscles – both major and minor – are located in your upper back where they connect your shoulder blades to your spine. They are part of a group of muscles that form the shoulder girdle which holds your shoulder and shoulder blade stable. Thanks to your rhomboid muscles, you are able to lift and rotate your shoulder blades and pull them back. Rhomboid muscles also help you throw and pull, lift your arm overhead and rotate your torso.
Causes of Rhomboid Pain
Rhomboid pain is generally not serious and can be treated easily with physiotherapy. It may be caused by postures that round your shoulders forward, such as hours spent sitting in front of a computer, or by poor posture. This tires the muscles and they become tight, forming a rhomboid muscle knot in the back. In addition, you may feel rhomboid pain from sleeping on your side, rowing, pushups, throwing motions, pulling motions, working out with weights and injury.
You may feel rhomboid pain after carrying heavy bags or backpacks. In addition, if you have problems with your shoulder joints due to arthritis or myositis, it may affect the surrounding muscles.
Symptoms of Rhomboid Pain
You generally feel rhomboid pain under the neck between the spine and shoulder blades. It may be referred to as shoulder blade pain. You may also feel it at the backs of the shoulders or in the mid-upper back. Additional symptoms can include:
- loss of movement, or difficulty or pain when moving the muscle;
pain when breathing; - a popping or grinding noise when you move the shoulder blade;
- tightness, swelling, and muscle knots around the muscle; and/or
- tenderness in the upper back area.
Treating Rhomboid Muscle Knots
If you are feeling rhomboid pain, begin by treating it as you would any other muscle injury – with RICE, or rest, ice, elevation and compression. Avoid activities that use these muscles; ice the area several times a day for 15 to 20 minutes; wrap the area with a compression bandage; and when lying down or sleeping, keep your chest and shoulders elevated with pillows. You can also use topical pain relievers, such as Voltaren, or essential oils to reduce pain.
After a few days of icing the area, you can apply heat with a warm compress or a heating pad for 15 to 20 minutes at a time; you may wish to alternate heat and ice.
If you’ve taken these steps and haven’t found relief, it’s time to see a physiotherapist. They can recommend a course of exercise that will help the injured area heal. These exercises may include stretching your chest to reduce the strain being placed on the muscles and those that strengthen your upper back.

You can also try a self massage: Take a tennis ball and place it between your upper back and the wall. Lean into it until you find the sore spot; then, gently make small circles with the ball. You can also lie on the floor and roll your shoulders over a foam roller to loosen and massage the muscles. Your physiotherapist will suggest other exercises targeted to your injury, depending on its severity.
It will take a bit of time to recover from rhomboid muscle pain, depending on how severely you have strained the muscles. Mild strains generally heal within three weeks, while more severe strains may take several months to heal.
Preventing Rhomboid Pain
Once your rhomboid pain is going, going, gone, keep it at bay by using a number of preventive measures:
- Always warm up before a workout and cool down afterward;
- Avoid lifting heavy objects, and use proper form when you do;
- Carry heavy backpacks on both shoulders, not one;
- Exercise and stretch regularly to stay in shape;
- Maintain a healthy weight;
- Practise proper technique when playing sports;
- Practise good posture while sitting, standing and walking;
- Take a break from exercise and activities when you feel sore or tired;
- Take frequent breaks to move around, walk, and stretch during periods of extended sitting; and
- Use protective equipment for sports and work.
Once you’re back to your old self, you can also consider working with your physiotherapist on an exercise program to ensure that you avoid imbalances in your body.
Soleus Muscle Pain
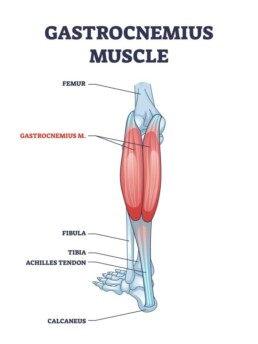
If you are diagnosed with a soleus muscle strain (a tear), you may wonder, “What is the soleus muscle?” You’re not alone. The soleus, one of the muscles that makes up the calf muscles, is not as well known as its partner, the gastrocnemius muscles that shape our calf. Soleus muscle pain can be felt as deep soreness or tightness when you press on your Achilles tendon, walk on your tiptoes, or pull your toes toward your shin.
The Soleus Muscle Explained
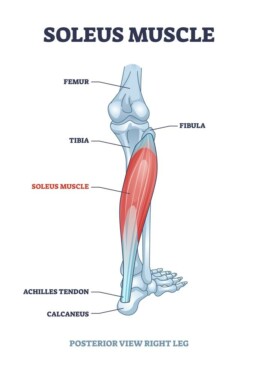
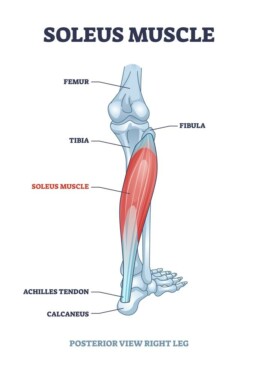
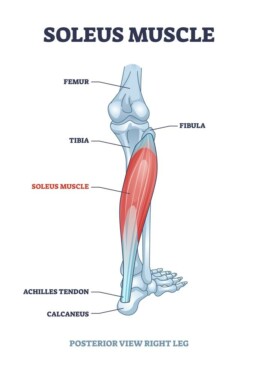
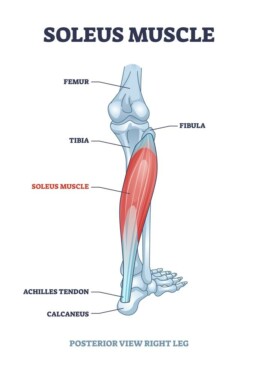
The name soleus is derived from solea, the Latin word for sandal, appropriate given the muscle’s placement. The soleus muscle is hidden beneath your two-heads of gastrocnemius muscle in your lower leg. It starts at the tibia and fibula bones and combines with the gastrocnemius at the heel to form the Achilles tendon. It is a broad, flat, powerful muscle that is important to maintaining posture and balance; it prevents you from falling forward at the ankle when you are standing and also helps control pronation, or the tendency of your foot to land on its outer edge, rather than plant itself squarely on the ground.
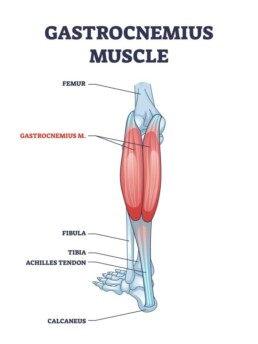
The soleus works with the gastrocnemius to enable plantar flexion, or the ability to point the toes downward; it is largely in charge of plantar flexion when you stand on your toes. It is also known as the soleal pump because it, with assistance from other muscles, pumps deoxygenated blood back from your legs to your heart.
The soleus muscle comprises mostly slow twitch muscle fibres and it is relatively resistant to fatigue, making it valuable in endurance activities such as distance running and walking. However, it is also occasionally involved in explosive movements, so it comes into play in sports such as basketball and tennis.
Causes of Soleus Muscle Pain
Soleus Muscle Pain When Walking
The soleus muscle, along with the other calf muscles, bears a heavy load when you run or walk; it supports a load that is between five and seven times your bodyweight. That’s a lot of pressure! If the soleus muscle fibres aren’t strong enough for the task at hand, it can cause muscle fatigue and tightness in the calf area. In fact, the soleus is one of the most common causes of pain in the calf area.
The soleus muscle is also subject to strain (i.e., tearing). This is generally due to a sudden overload to the muscle, such as a sprint or stepping off a curb, or to repetitive overuse. When there is an acute overload, you will feel soleus muscle pain when walking but may still be able to continue with the activity.
Soleus Muscle Pain Running
This type of strain is most common in sports with sudden acceleration and changes in direction, such as sprinting. It is especially prevalent when someone in a stationary position puts on a sudden burst of speed, as in basketball or football.
When the injury is due to repetitive overuse, the pain will build gradually over time, especially if the muscle is tight. Once it reaches that threshold, the more you continue the activity, the more it hurts. This is an injury common to runners.
When you strain your soleus, you have essentially pulled the muscle beyond the limit of its elasticity, stretching it too far and tearing some of the muscle fibres. The pain may be intense and the area may be tender to the touch, accompanied by bruising and swelling. Walking may be difficult.
Soleus Muscle Pain Treatment
You should begin treatment for your soleus as soon as you feel pain. Initially, you should implement the RICE method: Rest, Ice, Compression and Elevation.
Rest is essential to allowing the injury begin to heal. Depending on its severity, the injury will need rest for two to three days up to as much as two to three weeks.
Apply ice to the injured area for 10-to-15-minute periods at a time, three or four times daily. Don’t put ice directly on bare skin; wrap it first. When not applying ice, wrap the area with a compression bandage, although take it off at night. It will help reduce any swelling and provide support so you don’t injure the soleus further. With regard to elevation, this is most important during the first few days after injury, since keeping your calf raised above the level of your heart draws excess fluid away from your calf.
Next, consult with a registered physiotherapist for a complete evaluation of the injury and the most effective treatment regimen. He/she may suggest that you wear heel pads to keep the heel raised and decrease tension on the muscle. They may also suggest crutches or a rigid boot; it will depend on the severity of the injury.
Your physiotherapist will also suggest a course of exercise to strengthen the muscles so they can heal without being overloaded. They may also prescribe resistance exercises to help the muscle fibres align properly and balance exercises, since a soleus tear can leave you a bit unbalanced.
Strengthening Your Soleus
You can strengthen your soleus muscle as a means of preventing injury. The best options are seated single-leg and double-leg calf raises done with knees bent. You point your toes downward while your knees are bent, preferably at a 90-degree angle. (If you don’t bend your knees, the exercise will target the gastrocnemius muscle instead.)
You can also do standing heel raises by bending your knees about 30 degrees, lifting your heels off the floor and lowering them back down without turning the foot outward.
Treat your soleus muscle with care; it is a vital piece of your anatomy, whether you are a runner or simply aim to get from one place to another!
Intramuscular Stimulation (IMS)
If you’ve been experiencing chronic pain or tight muscles, intramuscular stimulation might offer relief. First, however, you might want to know a bit more about this technique, used by specially trained physiotherapists.
Origins
Intramuscular stimulation is actually a made-in-Canada solution to muscle tightness or pain. It was invented in the 1970s by Dr. Chan Gunn, a physician working for the BC Worker’s Compensation Board. Gunn was trained in Western medicine, but he was also adept at acupuncture, an ancient Chinese practice. He drew from both approaches to pain in creating IMS. It is based on the theory that much chronic pain results from the nerves overstimulating the muscles. IMS works to reset these nervous impulses as a way of reducing pain by using acupuncture needles to stimulate the affected muscles.
How Does IMS Work?
IMS releases or lengthens affected muscles so that they relax. Your IMS-certified practitioner will assess you to determine which, if any, muscles can be helped by this approach. They then sterilize the affected area and insert very fine needles – the same type of needles used for acupuncture – into a muscle and manipulate the depth and direction to stimulate healing. (The inserted needle targets a compressed nerve root.)
The needle causes the muscle to twitch or cramp in response, triggering a spinal cord reaction; once that occurs, the needle is removed. (If the muscle is functioning normally, it won’t twitch or cramp.) The muscle can then relax and begin to function normally. Dry needling, as it is called, also creates a tiny wound in the muscle that promotes blood flow to the area and stimulates healing by producing a healthy inflammatory response that removes toxins from the area.

How Does Intramuscular Stimulation Help?
Intramuscular Stimulation provides two major types of positive results: increased movement and significant pain reduction. As you progress through your treatment regimen, the tight bands of muscle will loosen and allow for increased joint mobility. In addition, as the muscle loosens, there will be less pressure and compression on your joints, nerves and ligaments, so your pain should subside.
Generally, depending on the duration of the pain, the tight or painful muscle will require a series of IMS treatments before the pain disappears or lessens to a great degree.
When Is IMS Appropriate?
IMS targets chronic musculoskeletal pain. It does not work for chronic inflammatory pain or other types of pain, such as pain from cancer, diabetes or degenerative neurological conditions such as Parkinson’s disease. IMS is usually not administered during pregnancy or to patients who have had surgery in the past 12 weeks. It has successfully been used to treat such issues as:
- Achilles Tendonitis
- Carpal Tunnel Syndrome
- Chronic postural pain
- Golfers and Tennis Elbow
- Chronic Tendonitis or Bursitis
- Headaches
- Iliotibial Band Syndrome Jaw and TMJ Pain
- Low Back Pain
- Myofascial Pain Syndrome
- Neck Pain
- Patello-femoral Syndrome
- Plantar Fasciitis
- Piriformis Syndrome
- Repetitive Strain Injuries
- Sciatica
- Shin Splints
- Shoulder and Hip impingement syndromes
- Spinal Disc Problems
- Torticollis Trigger Finger
Will IMS Be Painful?
IMS is generally considered to be unpleasant, but not painful – especially given the results. Each needle is only inserted for a few seconds, but as the muscle is stimulated into relaxation, there may be a bit of discomfort before the pain dissipates. Pain relief may happen quickly or it may take a few days. In addition, patients generally have increased movement and muscle function as a result. The IMS-trained physiotherapist carefully identifies the points for needle insertion so that the affected muscles can react.
Afterward, you may experience some bruising and soreness in the area. Your physiotherapist may recommend that you avoid vigorous exercise or stress to your body so the treatment can take effect. Drinking a lot of water and applying heat to the area will flush the body and assist in healing.
Acupuncture Compared to IMS
Acupuncture and IMS both use the same needles and dry needling technique, but they are very different therapies.
Acupuncture is an ancient Chinese medicine technique that focuses on using needles to stimulate the body’s meridians of energy, specifically those related to a certain organ or muscle. A series of needles is inserted around a particular point and may be left there for 10 to 20 minutes to effect change.
IMS, a technique that is only about 50 years old, blends Western medicine with traditional Eastern medicine to impact chronic pain and muscle dysfunction. It is based on Western medicine’s understanding of the human body’s physiology and anatomy.
Acupuncture is relaxing, but IMS can often be intense. However, both strive to help the patient feel better.
Coping with Posterior Shin Splints
While you may think of splints as devices used to immobilize injured body parts, it’s a term that has another connotation in the medical world, one with which many runners are all too familiar. Shin splints is a term used to describe pain in the lower leg; it refers to the inflammation of one of the muscles that runs along the tibia or shin bone, the tibialis posterior. The tibialis posterior runs along the inside rear of the tibia bone. Posterior shin splints are the most common cause of painful shin bones.
The Mechanics Behind The Pain
Your tibialis posterior muscle controls a portion of the foot’s arch when it is doing weight-bearing exercise. It helps to produce the motion that allows your foot to lift off the ground when you are running or walking, necessary to keeping the foot and ankle stable; this is called supination. The tibialis posterior muscle also helps to apply the brakes to the flattening of the arch when you are in motion.

What Causes Shin Splints?
Posterior shin splints can be result from various causes, including:
- Flat feet – Flat feet can put too much stress on the tibialis posterior muscle and tendon by causing the muscle to be lengthened. If the foot’s core muscles aren’t strengthened, the foot may be subject to over-pronate and there may be an inward knee collapse, which aggravates shin splints.
- Overuse or overtraining – If you increase your mileage on the roads, you are landing on your foot more often, which increases the force on your arches. If you run faster, you increase the force with which you strike the ground, which can also have a negative impact on your tibialis posterior muscle.
- Tight calf muscles – If your calves are tight, your ankle’s range of motion becomes limited, causing pronation that causes your tibialis posterior to work too hard.
- Weak hip and core muscles –
These muscles help control the leg’s inward rotation, and if the pronation becomes more extreme, it can aggravate your tibialis posterior muscle. - Worn out footwear – Walking or running shoes help support the feet and ankles, so if a shoe begins to break down, the foot may pronate more and require the tibialis posterior to work harder, which can lead to inflammation.
Symptoms of Posterior Shin Splints
- Dull, aching pain in the inside-rear front of the lower leg;
- Shin pain along the side of the tibia bone or within associated muscles; or
- An area that is tender to the touch.
However, you should talk to a registered physiotherapist or a physician before proceeding with specific treatment options. A physiotherapist will base the treatment on the severity of the injury.
With stage one shin splints, your pain disappears during warm up exercise, so you may be allowed to continue exercising unless the injury worsens. A stage two injury means the pain may reappear at the end of a workout, so your physiotherapist may recommend modified workouts while you are treated.
If shin pain worsens during a workout, this means that it’s time to suspend activity before the tibia suffers stress fractures. This is a stage three injury. If you have pain and discomfort all the time, your injury has progressed to stage four and it’s time to stop all activity. You may need crutches or an air cast to take pressure off the area while it heals.
It’s important to address shin splints even though the recovery isn’t quick; it usually takes at least two months. However, depending on the severity of the injury, you may be able to continue with modified exercise.

Diagnosis and Treatment
As with most injuries, it’s useful to start with the RICE method of treatment: rest, ice, compression and elevation. Apply ice every two to four hours for 20 to 30 minutes. Avoid anti-inflammatory drugs for the first 48 to 72 hours. See your physiotherapist as soon as possible to obtain a diagnosis so that you can begin to rehabilitate your injury. Initially, your physiotherapist may do some supportive taping to help support the injured soft tissue and offer your tibia some stress reduction.
Next, your physiotherapist will work with you to help you regain your full range of motion without pain. This often involves remoulding scar tissue so it doesn’t tear easily in the future by lengthening and orienting it through stretching, massage and targeted exercises. Your physiotherapist will also evaluate your gait to determine what corrections need to be made so that you can prevent a recurrence of your shin splints. You may need to wear corrective orthotics to give your foot some assistance.
Restoring strength to your muscles is also critical, so your physiotherapist will help you create a realistic exercise plan that will restore weakened calf, shin, quadriceps, gluteal and other lower limb muscles to their appropriate strength. Once you’ve reached this point, it’s time to return to your usual activities – but you’ll want to work with your physiotherapist to create a workable re-entry plan.
So, if you’re feeling pain in the area near your tibia, don’t hesitate to have it diagnosed. As they say, shin up – or do I mean chin up?!
Pulled Butt Muscle | Gluteal Pain
The phrase “Pain in the Butt” is a slang reference to someone who is annoying, but it derives from a real medical problem: a pulled or torn muscle in the buttocks that can, indeed, be painful.
What Causes Pain in the Gluteal Muscles?
One of the major causes of buttocks pain is a strain – a tear to one of the gluteal muscles. This type of injury is often called a pulled butt muscle. A strain happens when the load placed on the muscle exceeds its normal boundaries. It can result when there is too much force or repetitive force during the muscle’s contraction. They are most likely to occur during exercise, especially sports that involve running or jumping.
A strain, or tear, to a gluteal muscle, may result in sudden pain after a fall or an exercise session. Chronic wear and tear can also lead to a strain in the glutes. Your muscles may experience fatigue if you aren’t properly conditioned to handle a specific exercise or motion or a strain may result if you don’t warm up adequately before exercise. In addition, poor technique can lead to gluteus strains.
The Gluteus Muscles Explained
Your buttocks are medically referred to as your gluteus and each buttock comprises three separate muscles: gluteus maximums, gluteus medius and gluteus minimus – along with fat. These muscles run diagonally from the pelvic rim toward the femur, or thigh bone. They exist in layers with the gluteus minimus being the smallest and deepest; the gluteus medius in the middle and the gluteus maximus the most superficial. The three muscles work together to stabilize the pelvis and allow for hip motion by contracting or shortening.
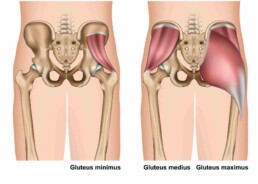
- The gluteus maximus is one of the body’s strongest muscles and is responsible for a leg extending backward. In one’s gait, it is crucial to pushing off and it is the muscle that allows you to straighten your hips when rising from a chair or ascending a flight of stairs.
- The gluteus medius muscle is responsible for the sideways movement of the leg (abduction) and in keeping your hips level when you move from side to side. It also helps steady your thigh bone when you run, jump or walk.
- The gluteus minimus muscle assists in sideways motion and internal rotation of the leg and helps the gluteus medius in stabilizing the hip and pelvis when one leg is lifted.
Symptoms of Buttock Pain
If the injury results from trauma, you may feel a sharp, sudden pain when it occurs. However, it will be most noticeable when you undertake activities that rely on the use of the affected gluteal muscle. Depending on the severity of the tear, your symptoms may include:
- A deep ache in your hip or buttock;
- Severe pain in the buttock;
- Difficulty climbing stairs;
- Unstable feeling in hips;
- Tingling and numbness in your buttock;
- Swelling or bruising in the hip and buttock area; and/or
- Sharp pain when squeezing your buttocks together.
Diagnosis and Treatment
If you experience gluteal pain and can pinpoint the time of an injury, be cautious for the first 48 to 72 hours. Rest is important. You may also want to ice the affected area using a bag of frozen peas or crushed ice wrapped in a damp towel. Apply the ice for 15 to 20 minutes each hour or two.
Until you receive treatment, it is important to proceed cautiously so the injury doesn’t worsen; avoid the temptation to stretch and exercise through the pain. This means avoiding certain motions and activities, such as sitting cross-legged or with your thigh crossed over; sitting in a deep chair; climbing stairs; and, of course, running or cycling.
You will also want to contact a licensed physiotherapist to assess your injury. A physiotherapist will stress and stretch your soft tissues, exploring the muscle strength, lengths, range of motion, flexibility and stability to determine the extent of the strain. They may ask for a diagnostic ultrasound, since this test shows soft tissues and tendons.
Your physiotherapist will start rehabilitation with movements involving the specific muscle before moving on to resisted movements, followed by activities that involve the muscle, such as climbing stairs. Then, you can transition to running and jumping activities. Exercises will focus on strength and range of motion.
It is important to treat a gluteal strain or pulled butt muscle, because if it doesn’t heal properly, it can recur and become a chronic problem. Generally, for a moderate tear, you can expect healing to take place within six to eight weeks. If the strain is a recurring one, it will take longer.
Take heart! With determination and treatment, you will no longer be the butt of jokes about your gluteal strain.
Shoulder Pain After Sleeping
There are multiple reasons why many people don’t get enough sleep at night. One of the main reasons is physical discomfort, which can be due to inadequate neck support or a room temperature that’s too warm or too cold. Often, the cause of lack of sleep due to physical discomfort is shoulder pain.
There are several conditions that can cause shoulder pain during and after sleeping. One common cause is an injury to the rotator cuff. The rotator cuff is a group of muscles and tendons that are attached to the bones of the shoulder joint. These muscles and tendons allow you to move your shoulder while at the same time keeping it stable. An injury to the rotator cuff can be caused by tendonitis, strains, or partial or complete tears.
Can Sleeping On Your Side Cause Shoulder Pain?
Tendonitis occurs when muscles in the shoulder are injured or overused, causing inflammation. An inflamed shoulder is painful. The pain can be felt during the day, at night, or both. Tendonitis is caused by keeping the arm in the same position for long periods of time, such as sitting at a computer all day. Another cause is sleeping on your side at night, which can cause your arm to fall asleep. Other causes of tendonitis are sports injuries, poor posture, tears, and aging.
Rotator Cuff Tears
Rotator cuff tears can be caused by a single event or by repeated motion over time that eventually results in a small tear that can grow bigger over time – think of baseball pitchers and their repetitive arm motion. Besides rotator cuff injuries, other conditions that cause shoulder pain are osteoarthritis, bursitis, and shoulder impingement:
Osteoarthritis
In this condition, the cartilage — the material that provides cushioning to the ends of bones — degrades. Degradation of cartilage in the shoulder joint causes shoulder pain over time. Osteoarthritis occurs with age as well as from trauma and injury. Symptoms include a decreased range of motion in the shoulder joint and stiffness and pain with movement. You may also hear clicking or grinding sounds in your shoulder when you move it.
Bursitis
Bursae are fluid-filled sacs that cushion tissues around joints. Shoulder bursitis occurs when the bursae around the shoulder joint become inflamed or irritated. Symptoms include redness and stiffness in the shoulder, local tenderness, and increased pain from movement or pressure.
Shoulder Impingement
Shoulder impingement occurs when the tissues that surround the rotator cuff grind or rub against adjacent bones and tissues. This rubbing can eventually lead to bursitis, tendonitis, or bone spurs. This condition is characterized by weakness in the shoulder and pain at the top or outer part of the shoulder.
Prevention and Treatment of Nighttime Shoulder Pain
The duration of your shoulder pain from sleeping depends on your sleeping posture, as well as on your underlying medical conditions. Here are some things you can do to prevent waking up with a sore shoulder:
- Avoid applying direct pressure on your shoulder while sleeping. Sleeping on your side, sleeping with your arm under your pillow, or sleeping with your elbow above your head can irritate the rotator cuff and cause discomfort during sleep, especially if you sleep on the same side every night. You can wake up with a dull pain or ache in the shoulder and have a reduced range of motion due to stiffness.
- If you sleep on the shoulder that hurts when you wake up, try switching sides when you sleep to give your sore shoulder a break while your opposite shoulder supports your body during sleep. You can also sleep on your back so that your body weight is more evenly distributed and you’re not putting any stress on your shoulders.
- Regular exercise strengthens the muscles and tendons in your shoulders, neck, and spine by helping to increase range of motion and strengthen your upper body, including the rotator cuff. A physiotherapist can help prescribe appropriate exercises for you.
- Add or remove pillows to support your body and shoulders.
How To Relieve Shoulder Pain After Sleeping
Applying heat and cold is a natural way to relieve pain in your shoulder after sleep.
- If you have osteoarthritis, apply moist heat to the shoulder joint to ease stiffness and relax muscles.
- For a strained shoulder, first apply ice to reduce inflammation and pain, then apply heat to reduce stiffness.
- If you have tendonitis in your shoulder, apply ice to reduce inflammation and pain.
- If heat and cold don’t relieve your shoulder pain, you can consider taking non-steroidal anti-inflammatory drugs for temporary pain relief, such as acetaminophen, NSAIDs, or Naproxen.
When to See a Doctor
For most people, shoulder pain after sleeping resolves within 48 hours. For some people, however, the pain becomes persistent. If self-help measures don’t work, it’s time to see a physiotherapist.
If your shoulder hurts longer than a few weeks, if you have additional pain or limited movement, and if you regularly wake up at night because of your shoulder pain, it’s time to consult your doctor.
Other signs that indicate a need for medical attention are grinding, snapping, clicking, or popping noises in your shoulder; visible growths or masses in your shoulder; and an inability to perform your regular tasks of daily living.
Physiotherapy for Pain Management
Usually, the last thing you want to do when you’re in pain is move. It feels much more comfortable to take a painkiller and sit still so the pain seems less. However, sitting still may be the worst thing you can do if you have chronic pain because it causes you to become weaker in the long term. That’s where physiotherapy for pain management comes in.
Physiotherapy for Pain Management
Physiotherapists specialize in teaching you how to move in ways that are safe, yet functional, so you don’t lose body strength. Physiotherapy is effective for pain due to osteoarthritis, rheumatoid arthritis, fibromyalgia, and neuropathic pain (caused by injured nerves or tissues). Physiotherapy works for pain that affects the knees, neck, head, back, and shoulders. It works for both acute and chronic pain (pain you’ve had for more than 3 months).
Pain Management Treatment Options
Physiotherapists offer a variety of treatments that may include:
- movement therapy and corrective exercise, such as treadmill walking or walking in a swimming pool;
- massage;
- bone and joint manipulation and mobilization;
- acupuncture;
- manual therapy and stretching using the hands and tools on soft tissue;
- electrotherapy, such as TENS (transcutaneous electrical nerve stimulation);
- posture awareness and correction or improvement;
- cold or heat packs;
- cold laser therapy, which reduces inflammation and pain by releasing endorphins, the body’s natural painkillers;
- help with understanding the cause of your pain;
- education and advice on how to manage pain while doing daily activities;
- breathing, relaxation, and mindfulness; and
- self-management strategies on pacing, sleep, and stress.
- movement therapy and corrective exercise, such as treadmill walking or walking in a swimming pool;
- massage;
- bone and joint manipulation and mobilization;
- acupuncture;
- manual therapy and stretching using the hands and tools on soft tissue;
- electrotherapy, such as TENS (transcutaneous electrical nerve stimulation);
- posture awareness and correction or improvement;
- cold or heat packs;
- cold laser therapy, which reduces inflammation and pain by releasing endorphins, the body’s natural painkillers;
- help with understanding the cause of your pain;
- education and advice on how to manage pain while doing daily activities;
- breathing, relaxation, and mindfulness; and
- self-management strategies on pacing, sleep, and stress.
How Does Physiotherapy Help With Pain?
Physiotherapists work with patients individually to pinpoint and understand each patient’s pain and what caused it. Before deciding on a treatment plan, a physiotherapist will do a thorough assessment of your pain situation. They will choose a certain therapy or therapies based on the degree and nature of your pain as well as on your physical ability. They will then determine how best to manage your pain.
The advantage of seeing a physiotherapist for pain management is that they are able to spend time with you to ask questions, discuss your pain issues with you, and obtain feedback from you while you do your exercise routine, something that regular doctors may not have time for.
What Results Can I Expect?
If you do your prescribed exercises three-to-four days each week for 30 minutes a day, your chronic pain will improve because you’ll have:
- increased muscle strength;
- greater joint stability;
- more endurance; and
- more flexible joints and muscles.
Consistency Is Important
It’s important to be consistent with your exercise routine. Regular exercise not only helps you to maintain your ability to move and function, it also helps your body to heal itself by increasing endorphins, your body’s natural pain-relieving chemicals.
The more you move, the less pain you’ll have in the long term. This is essential. It is important to understand that, ultimately, you have to do the work if you want to feel better. A physiotherapist can only guide you to a faster and more complete recovery.
With the help of a physiotherapist, you will learn how to exercise safely to accommodate your pain. As a result, you’ll be able to function better on a daily basis.
Pain Management Is A Team Effort
A physiotherapist is an invaluable member of your healthcare team when it comes to pain management. You may also need a regular physician, in case you need medication to help manage your pain, and a clinical psychologist to help you deal with your pain better on a mental-emotional level.
If you’re in chronic pain, seeing a physiotherapist as a member of your healthcare team will reduce your pain levels and improve your quality of life.
What Is Post-Operative Rehab Physiotherapy?
Surgery is not something to take lightly, because it places stress on your entire body: not only on the bones, muscles and soft tissue involved, but also on the heart, the lungs, the circulatory system and other organs.
Problems that may arise following various types of surgery include issues with balance and posture; breathing difficulties; loss of sensation; weakness; reduced lung function; blood clots; and incontinence.
Given the impact, it’s not surprising that your body needs time to recover its strength and stamina, as well as its mobility. In order to give your body the best opportunity to adjust to the demands of surgery and achieve the results you envision, you’ll want to take advantage of post-operative rehab physiotherapy.
Benefits of Post-Operative Rehab Physiotherapy
A licensed physiotherapist will be able to promote healing, help improve your range of motion in the affected area, prevent the loss of muscle mass and keep scar tissue from forming. Physiotherapy assists you in achieving optimal post-operative physical functioning. In addition, it helps to keep you motivated and reduce the normal post-operative feelings of stress and frustration.
Post-operative physiotherapy is always beneficial, and it is often recommended for surgeries such as:
- Knee, e.g., replacements, arthroscopy, fractures, meniscal repairs;
- Hip, e.g., replacements or resurfacing, fractures;
- Shoulder, e.g., reconstruction, rotator cuff repair, stabilization;
- Ankle and foot, e.g., spur removal, reconstruction, ligament repairs;
- Spine, e.g., fusion/stabilization; and
- Elbow, e.g., releasing tennis or golf elbow
In fact, research has demonstrated specific benefits of post-operative physiotherapy for a number of procedures:
- Total hip and knee replacement: earlier hospital discharge;
- Cardiac surgery: lung function;
- Spinal surgery: improved spinal mobility;
- Colorectal surgery: increased cardiovascular fitness;
- Breast surgery: fewer side effects; and
- Many surgeries: reduced risk of blood clots.
Your first encounter with post-operative physiotherapy will generally take place in the hospital, where the staff physiotherapists often provide basic rehabilitation at the bedside to:
- Prevent breathing and vascular complications;
- Offer movement assistance; and
- Assist you with the use of necessary mobility aids.
Phases of Post-Operative Rehab Physiotherapy
Once you are discharged, you’ll want to continue your recovery under the care of a licensed physiotherapist. Your licensed physiotherapist will work collaboratively with you to create a rehabilitation program designed to meet your goals and needs. They will conduct a full assessment and take into account the restrictions and timelines specific to the type of surgery you’ve undergone. Post-operative physiotherapy happens in three phases, each with a different focus: early recovery, returning range of motion and restoring function.
Early Recovery Phase
The early recovery phase of rehabilitation begins once there is a reduction in post-operative pain and swelling. Initially, they will generally work with you to further alleviate any pain and swelling, suggest gentle exercises to begin restoring muscle function and provide manual therapy to start increasing range of motion.
Returning Range of Motion Phase
Once you’re ready, your licensed physiotherapist will move on to help you normalize your body’s range of motion, strength and mechanics. Your program during this phase of physiotherapy will likely include balance and proprioception – the sense of your body’s position in space – exercises, more challenging strengthening exercises, soft tissue treatment for mobility and more aggressive manual therapy that will help restore range of motion.
Restoring Function Phase
The final phase of your rehabilitation will focus on restoring independent movement, continuing to build your strength and meeting your personal goals. Each person is different; one may be hoping to be involved in competitive sport, while another may simply want to be able to keep up with energetic young children or grandchildren. Therefore, the exercises during this phase of your program will be targeted toward complex functional goals. Your balance and proprioception exercises will also increase in difficulty and manual therapy will continue to increase your range of motion.
By taking advantage of the services offered by a licensed physiotherapist, you are giving your body the boost it needs to function at its best.
Why Physiotherapy is Important in Sports
As 2021 gets underway, thousands of us have undoubtedly made New Year’s resolutions to up their exercise quotient and get fitter. Unfortunately, in our eagerness to do so, we may overexert themselves and cause injuries. Luckily, there are physiotherapists to help put us back together again, unlike poor Humpty Dumpty in the famous nursery rhyme.
Physiotherapists are experts at evaluating, restoring and maintaining physical function and mobility. They also can assist individuals in achieving optimal performance. Since sports are all about motion and performance, sports physiotherapists are the ideal resource for athletes to draw upon, whether they are injured or simply seeking to improve their performance.
Think about the last time you watched your favourite sports team play. Undoubtedly, at some point, play was stopped because a player had sustained a possible injury. Out onto the field of play comes the trainer, who is often a trained physiotherapist, to evaluate the injury and help determine whether the player can continue the game without doing irreparable damage.
Why is Sports Physiotherapy Essential for Athletes?
The physiotherapist’s goal is to speed up healing and to help the athlete return to action as quickly as possible with the proper combination of therapy and exercises.
Of course, it’s not only professional athletes who can benefit from sports physiotherapists. We amateurs get injured regularly and are eager to find our way back into action and prevent the injury from recurring. Physiotherapists not only consider our injuries; they look at the underlying causes so that their treatments benefit the entire body.
Here are some of the ways sports physiotherapy can assist athlete, whether professional or amateur:
-
- Improving joint and muscle flexibility. Flexibility is a key to optimal performance. Physiotherapists can provide exercises that will improve flexibility to help you meet your sports goals, whether you’re working toward a tournament or simply trying to improve your fitness.
- Enhancing strength. Sports physiotherapy improves your ability to deal with physical stress, something that is an integral part of many high-contact sports. The stronger your body, the less susceptible it is to injury.
- Preventing injury. Participants in different sports are susceptible to different injuries. A sports physiotherapist can suggest an exercise regimen designed to strengthen your body accordingly. They will also advise you about proper warmups and sensibly increasing your physical workload.
- Assisting with relaxation. After intense exercise, it may be hard for you to relax and wind down. A physiotherapist can assist you with stretching and healing, and the clinic may also offer massage therapy to help your sore muscles. Soon, you’ll have the energy to carry on.
- Rehabilitating injury. Everyone gets injured once in a while, no matter how careful they are. Sports phyisotherapists evaluate your injury and determine a course of treatment (exercises, acupuncture, etc.) that will help you heal as quickly as possible and strengthen the appropriate areas to help prevent the injury from recurring.
- Managing pain. Physiotherapists can offer you a number of exercises and techniques designed to reduce pain and discomfort. They also help athletes handle chronic conditions that can interfere with workouts.
What to Expect at a Physiotherapy Session
If you’ve never been to see a physiotherapist, there is a standard approach to your injury or concern that you can expect.
Prior to suggesting any treatment, your physiotherapist will want to assess your condition. You’ll need to provide information about your medical history, your lifestyle, your medications and the sports in which you participate. If you have X-rays or other test information, they will want to see it. This is an opportunity for you to ask questions, too.
Once the physiotherapist has the necessary information, they will assess your injury. The assessment may include evaluation of your movement, your posture and your ligament stability.
Next, the physiotherapist will design a treatment plan to help you heal faster, achieve your performance goals or prevent injury. They will run through the exercises with you to ensure you know how to do them correctly.
You’ll be sent home to follow their plan, with regular visits to allow them to monitor your progress. You should be pleased at the progress you see if your follow the plan.
Remember, participation in sports comes with an inherent risk, so why not do all you can to minimize it while maximizing your potential?








